Introduction: Current COG protocols for childhood ALL recommend increasing 6-mercaptopurine (6MP) and methotrexate (MTX) dose intensity (DI=prescribed therapy dose/ planned protocol dose) to >100% during maintenance for patients exhibiting inadequate myelosuppression (surrogate for systemic exposure to 6MP/MTX). Whether increasing DI >100% (high DI) to achieve myelosuppression is associated with increased toxicity is not clear. Additionally, whether high DI influences relapse risk, and the direction of that association, remains unknown. Nonadherence to 6MP results in inadequate myelosuppression and prompts clinicians to increase the prescribed dose. Nonadherence to 6MP is also associated with relapse (Bhatia, JAMA Onc 2015). Prior literature examining the association between high DI and relapse risk did not consider adherence to chemotherapy. Here, we examined whether high 6MP/MTX DI affects toxicity or relapse, taking 6MP adherence into consideration.
Methods: We used data collected by COG-AALL03N1 (primary aim: 6MP adherence and risk of relapse) to examine the association between high DI and (i) hematologic toxicity, and (ii) relapse risk. Inclusion criteria: (i) age <21y at ALL diagnosis, (ii) receiving maintenance therapy in first remission and >6mo since starting maintenance, (iii) wild-type thiopurine methyltransferase ( TPMT) or nucleoside diphosphate-linked motif 15 (NUDT15) and (iv) objectively measured 6MP adherence for 6mo per patient (using MEMS-TrackCaps). 6MPDI and MTXDI were calculated monthly for 6mo. Updates on vital status, relapse or second neoplasm were collected every 6mo-1y from participating sites for up to 10y. Exposure: ‘high DI’ phenotype: (i) 6MPDI or MTXDI ≥110% at any time during the first 4 study months, or (ii) 6MPDI or MTXDI 100% to 110% at study enrollment and ≥25% increase over the first 4 study months. All other patients were categorized as having ‘normal DI’. Outcomes: (i) hematologic toxicity (absolute neutrophil count <500 cells/µL, platelet count <50,000 cells/mm 3, or treatment interruption due to low ANC/platelets) during the subsequent 2 study months (months 5 and 6); and (ii) ALL relapse any time after month 4. We used logistic regression to examine the association between high DI and hematologic toxicity, adjusting for age at study entry, sex, race/ethnicity. The association between DI and relapse was estimated using proportional sub-distribution hazard regression models, adjusting for age at study entry, blast cytogenetics, time from start of maintenance, and treatment interruptions. Analyses were stratified by 6MP adherence (adherers: median adherence ≥85%; non-adherers: median adherence <85%). Adherence was included in both models to account for residual confounding.
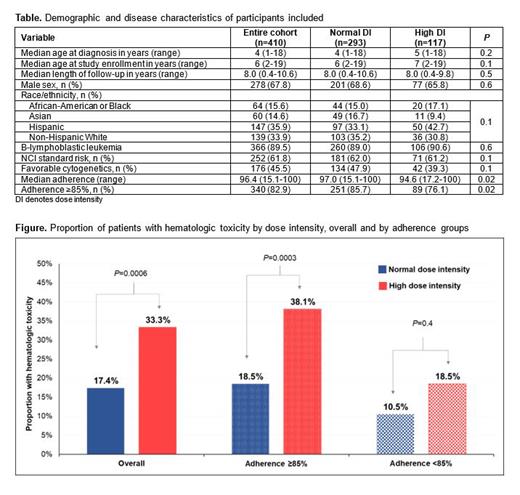
Results: Characteristics of the 410 eligible participants are summarized in the Table; the cohort was followed for a median 7.9y (range, 0.2-13). There were no significant differences between patients with normal (71.5%) vs high (28.5%) DI. Patients with high DI had lower median 6MP adherence (94.6% vs 97.0%, P=0.02). Hematologic DLT: As shown in the Figure, the proportion of patients with hematologic toxicities was significantly higher among adherers with high DI compared with adherers with normal DI (38.1% vs 18.5%, P=0.0003). In contrast, the proportion of patients with hematologic toxicities was not significantly different by DI status among non-adherers (18.5% vs 10.5%, P=0.4). Multivariable analysis revealed that high DI was associated with 2.9-fold greater odds of hematologic toxicity among adherers (95%CI=1.6-5.1, P<0.001) and a non-significant 2.1-fold greater odds of hematologic toxicity among non-adherers (95%CI=0.4-10.1, P=0.4). Relapse risk: The adjusted hazard of relapse among adherent patients exposed to high DI was 2.2-fold greater (95%CI=1.0-5.1, P=0.06) than adherent patients exposed to normal DI after adjusting for covariates. In contrast, the hazard of relapse among non-adherent patients exposed to high DI (vs. normal DI) was not elevated (HR=0.9, 95%CI=0.2-3.8, P=0.8).
Conclusions: High antimetabolite dose intensity in children with ALL who adhere to oral 6MP during maintenance therapy is associated with higher odds of hematologic toxicities as well as increased hazard of relapse. These findings inform clinicians about the issues related to dose escalation beyond protocol doses, especially among adherent patients.
Disclosures
Angiolillo:Servier Pharmaceuticals: Current Employment. Dickens:Amgen: Honoraria; American Society of Pediatric Hematology Oncology: Membership on an entity's Board of Directors or advisory committees; Iowa Cancer Consortium: Membership on an entity's Board of Directors or advisory committees; American Academy of Pediatrics: Membership on an entity's Board of Directors or advisory committees; Tempus Inc.: Honoraria; Syndax: Research Funding.